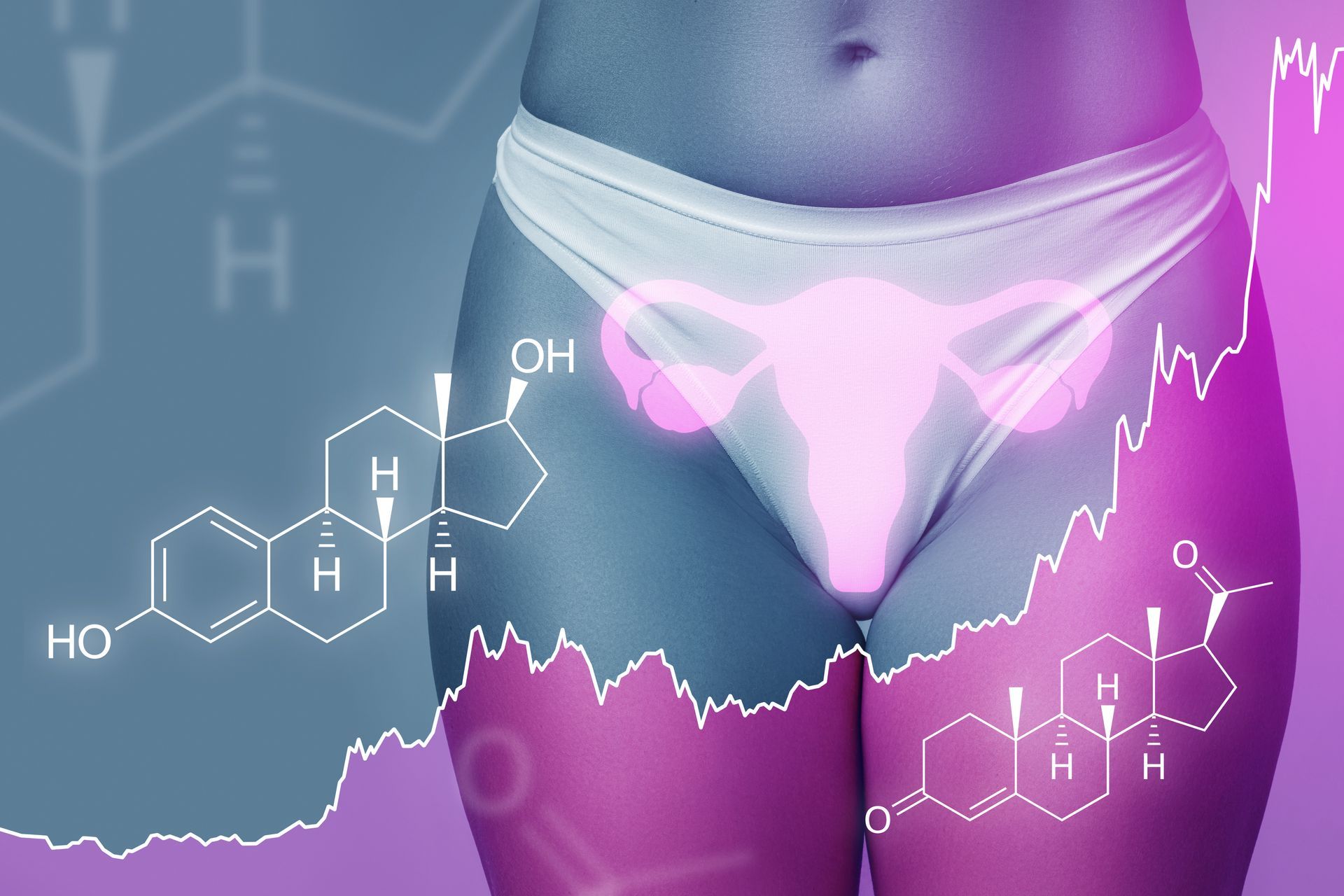
Menstration
Women's Health Care of New England • August 1, 2019
The menstrual cycle is a normal monthly cycle, occurring in women during their reproductive years, in which the lining of the uterus builds up to support a fertilized egg. If no pregnancy occurs, this extra lining separates, passes through the cervix, and is “your period.”
Day one of your menstrual cycle is the first day of your period, and women’s menstrual cycles can range from 21 days to over 35 days. As a woman approaches menopause, the time between periods gradually gets longer.
WHEN TO CALL YOUR OB GYN PROVIDER:
- Your period has stopped for 3 months or longer
- Periods less than 21 days apart or more than 45 days apart
- Severe abdominal or pelvic pain occurs during menstruation or sexual intercourse
- Menstruation has not started by the age of 16
- Menstrual bleeding is excessive (more than one pad or tampon per hour for several hours)
- Menstrual periods lasting longer than 7 days
- Bleeding or spotting between periods
- Fever, vomiting, or weakness occurs after using tampons
- PMS symptoms that are disrupting your life, or cause you to feel out of control
NORMAL MENSTRUAL BLEEDING
Periods usually last about 5 days. Some women have shorter periods and others have them longer. Heavy bleeding often is accompanied by clots and cramping.
The average blood loss from menses is a juice glass amount of blood, approximately 4 ounces or 8 tablespoons. It may be normal for some women to experience heavier bleeding, up to twice the “average” amount and still be within the normal range. Most sanitary products are saturated with 2 tablespoons (1oz.) of fluid.
Many women experience one “heavy” day during their period, but this is preceded and followed by lighter flow days. If at any time, you are experiencing consistent heavy bleeding, clots, cramping, and regularly soaking your sanitary protection once or twice an hour, you should contact your physician.
CRAMPS (DYSMENORRHEA)
To some degree, most women experience menstrual cramping in the lower abdomen, lower back, thighs, and hip areas. The pain does not dominate more on one side and the severity of symptoms varies between individuals. 1 in 10 women do experience severe cramping associated with diarrhea, nausea, vomiting, weakness, and headache.
Cramps come from contractions of the uterus, which is a smooth muscle. Menstrual cramps arise from the action of prostaglandin, a hormone on the smooth muscle of the uterus. Prostaglandin is abundant in the uterine muscle and increase in amount just before menses. These chemicals stimulate the uterus to contract, or cramp. As menstrual flow continues, the prostaglandin is released with the discharge. It tends to be that high flow days are crampiest, and then this subsides as the flow lightens.
RELIEF MEASURES FOR MENSTRUAL CRAMPS
Apply heat, either with heating pads against the lower abdomen or a weighty and warm hot water bottle against the crampy area.
Rest either with bent knees curled toward the belly, or supported beneath the knees with 1 or 2 pillows.
Analgesics, over the counter medication can be very helpful, but it is most beneficial if taken before the cramping symptoms increase.
Ibuprofen, along with other non-steroidal anti-inflammatory medications, has an action that decreases prostaglandin activity and relieves symptoms. There are cautions relating to its potential to be harsh on sensitive stomachs – so read the label of these products thoroughly and consult with your physician when necessary. Acetaminophen is another over the counter medication that has analgesic effects and may help to relieve symptoms.
Prescriptions for oral contraceptives have been shown to decrease cramping. Your health care provider can advise the best option for your specific needs.
We are pleased to let you know that two of our APRNs — Laury Berkwitt and Catherine Levins— have taken a keen interest in offering hormone replacement management. If you are experiencing symptoms of menopause or hormone changes, they are available to evaluate your needs and, if appropriate, prescribe hormone therapy (HRT) tailored to your care plan.

Happy St. Patrick’s Day from the WHCNE family! Wishing you a joyful and festive St. Patrick’s Day! At Women’s Health Care of New England, we celebrate the spirit of community and care. Our dedicated team is here to support you with quality, compassionate healthcare. Enjoy the day in good health and happiness!